Whether you are a healthcare professional, a patient, or simply curious about hematomas, this guide aims to provide you with valuable insights into the different types of hematomas and their implications. So, let’s begin our exploration of this fascinating yet potentially concerning medical condition.
Understanding Hematomas
A hematoma refers to a localized collection of blood outside the blood vessels, usually caused by an injury or trauma. It occurs when blood vessels rupture, leading to bleeding into the surrounding tissues. Hematomas can occur in various parts of the body, including the skin, muscles, organs, and even the brain.
Causes of Hematomas
Hematomas can be caused by a range of factors, including:
Trauma: The most common cause of hematomas is trauma, such as a fall, sports injury, or car accident. The forceful impact can damage blood vessels, resulting in bleeding and the formation of a hematoma.
Surgery: Hematomas can also develop as a complication of surgical procedures. During surgery, blood vessels may be inadvertently damaged, leading to bleeding and subsequent hematoma formation.
Blood Disorders: Certain blood disorders, such as hemophilia or thrombocytopenia (low platelet count), can increase the risk of hematomas. These conditions impair the blood’s ability to clot properly, making individuals more susceptible to bleeding and hematoma formation.
Symptoms and Diagnosis
The symptoms of a hematoma can vary depending on its location and size. Common signs and symptoms include:
– Swelling and inflammation in the affected area
– Pain or tenderness
– Discoloration of the skin (bruising)
– Limited range of motion
– Palpable lump or mass
To diagnose a hematoma, a healthcare professional may perform a physical examination and review the patient’s medical history. Imaging tests, such as ultrasound, CT scan, or MRI, may be ordered to assess the extent and location of the hematoma.
Treatment Options
The treatment of hematomas depends on their size, location, and severity. In some cases, small hematomas may resolve on their own without intervention. However, larger or symptomatic hematomas may require medical intervention. Treatment options include:
Observation: Small, uncomplicated hematomas may be monitored over time to ensure they resolve without complications.
RICE Therapy: Rest, ice, compression, and elevation (RICE) can help reduce swelling and pain associated with hematomas.
Drainage: In some cases, a healthcare professional may need to drain the hematoma using a needle or make a small incision to remove the accumulated blood.
Surgery: Surgical intervention may be necessary for large or deep hematomas that do not respond to other treatments. The surgeon will remove the hematoma and repair any damaged blood vessels.
Complications and Prevention
If left untreated or not managed properly, hematomas can lead to complications such as infection, tissue damage, or the formation of scar tissue. To prevent hematomas, it is important to take precautions to minimize the risk of injury, wear protective gear during physical activities, and follow proper post-operative care instructions.
Understanding the causes, symptoms, diagnosis, and treatment options for hematomas is crucial in effectively managing and preventing complications associated with these localized collections of blood.
Subdural Hematomas
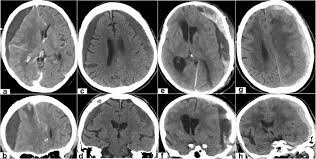
A subdural hematoma is a type of hematoma that occurs when blood accumulates between the dura mater (the outermost layer of the meninges) and the arachnoid mater (the middle layer of the meninges) in the brain. This condition is usually caused by a head injury or trauma that results in the tearing of blood vessels, leading to bleeding in the subdural space.
Acute Subdural Hematomas
Acute subdural hematomas are characterized by rapid bleeding and the accumulation of blood within the subdural space. This type of hematoma often occurs as a result of severe head trauma, such as a car accident or a fall from a significant height. The symptoms of an acute subdural hematoma can develop rapidly and may include severe headache, confusion, dizziness, nausea, and loss of consciousness.